DIGESTION OF DIETARY PROTIENS
Digestion of dietary proteins has two principle sites, which are gastric digestion and deudenal digestion but it usually starts in the stomach. Secretion of HCl activates formation of pepsin from pepsinogen which hydrolyses peptide bonds of dietary proteins to release aromatic amino acids. Similarly, in the small intestine digestion continues. Zymogens are activated for the breakdown of peptide bonds to release amino acids which are absorbed into the small intestine.
AMINO ACID DEAMINATION
Transamination is a process by which amino group is transferred to the keto acid to yield the keto acid of the original amino acid and a new amino acid, catalyzed by amino transferases. Glutamate is oxidatively deaminated in the mitochondrion and release ammonia.
THE UREA CYCLE
This cyclic pathway takes place in the liver, partly in the mitochondria and partly in cytosol. There is interrelation between urea cycle and citric acid cycle. Fumarate of the urea cycle is taken up by citric acid cycle. Carbamoyl phosphate synthetase I is the regulatory enzyme.
METABOLIC BREAK DOWN OF INDIVIDUAL AMINO ACID
Catabolism of amino acids gives rise to the intermediate compounds of citric acid cycle. Alanine, serine, cysteine and asparagine are converted to oxaloacetate. Glutamine, proline, arginine and histidine are converted to α- ketoglutarate through glutamate. Succinyl CoA is a point of entry for non polar amino acids like methionine, valine and isoleucine. Leucine is degraded to acetyl CoA and acetoacetate. Tryptophan, lysine, leucine, phenylalanine, tyrosine and isoleucine donate their carbons to acetyl CoA. Various disorders of amino acid catabolism are observed due to the defective enzymes. Tryptophan, tyrosine, glycine and glutamate are the precursors of some of the biologically important compounds. Biotin, Tetrahydrofolate or S-Adenosyl methionine is the enzyme cofactors in catabolism which transfer carbon compounds.
AMINO ACID BIOSYNTHESIS
Nonessential amino acids are formed from intermediates of carbohydrate metabolism. Alanine is formed from pyruvate and aspartate from oxaloacetate. Asparagine is formed from aspartate. Glutamate is formed from α ketoglutarate and glutamine from glutamate. Glutamate is the precursor of proline and arginine. Cysteine is synthesized from 3 – phosphoglycerate. During the process, serine is the intermediate compound which gives rise to glycine. Threonine is an essential amino acid. It is formed from β-aspartate. Methionine and lysine alsohave a common precursor. Valine, Leucine and isoleucine are formed from pyruvate. Phenyl alanine, tyrosine and Tryptophan are formed from phosphoenol pyruvate and erythrose – 4 – phosphate through the intermediate compound called chorismate. Histidine usually form L-glutamate.
Digestion of dietary proteins has two principle sites, which are gastric digestion and deudenal digestion but it usually starts in the stomach. Secretion of HCl activates formation of pepsin from pepsinogen which hydrolyses peptide bonds of dietary proteins to release aromatic amino acids. Similarly, in the small intestine digestion continues. Zymogens are activated for the breakdown of peptide bonds to release amino acids which are absorbed into the small intestine.
AMINO ACID DEAMINATION
Transamination is a process by which amino group is transferred to the keto acid to yield the keto acid of the original amino acid and a new amino acid, catalyzed by amino transferases. Glutamate is oxidatively deaminated in the mitochondrion and release ammonia.
THE UREA CYCLE
This cyclic pathway takes place in the liver, partly in the mitochondria and partly in cytosol. There is interrelation between urea cycle and citric acid cycle. Fumarate of the urea cycle is taken up by citric acid cycle. Carbamoyl phosphate synthetase I is the regulatory enzyme.
METABOLIC BREAK DOWN OF INDIVIDUAL AMINO ACID
Catabolism of amino acids gives rise to the intermediate compounds of citric acid cycle. Alanine, serine, cysteine and asparagine are converted to oxaloacetate. Glutamine, proline, arginine and histidine are converted to α- ketoglutarate through glutamate. Succinyl CoA is a point of entry for non polar amino acids like methionine, valine and isoleucine. Leucine is degraded to acetyl CoA and acetoacetate. Tryptophan, lysine, leucine, phenylalanine, tyrosine and isoleucine donate their carbons to acetyl CoA. Various disorders of amino acid catabolism are observed due to the defective enzymes. Tryptophan, tyrosine, glycine and glutamate are the precursors of some of the biologically important compounds. Biotin, Tetrahydrofolate or S-Adenosyl methionine is the enzyme cofactors in catabolism which transfer carbon compounds.
AMINO ACID BIOSYNTHESIS
Nonessential amino acids are formed from intermediates of carbohydrate metabolism. Alanine is formed from pyruvate and aspartate from oxaloacetate. Asparagine is formed from aspartate. Glutamate is formed from α ketoglutarate and glutamine from glutamate. Glutamate is the precursor of proline and arginine. Cysteine is synthesized from 3 – phosphoglycerate. During the process, serine is the intermediate compound which gives rise to glycine. Threonine is an essential amino acid. It is formed from β-aspartate. Methionine and lysine alsohave a common precursor. Valine, Leucine and isoleucine are formed from pyruvate. Phenyl alanine, tyrosine and Tryptophan are formed from phosphoenol pyruvate and erythrose – 4 – phosphate through the intermediate compound called chorismate. Histidine usually form L-glutamate.



![eC_{Cr} = \frac { \mbox{(140 - Age)} \ \times \ \mbox{Mass (in kilograms)} \ \times \ [{0.85\ if\ Female}]} {\mbox{72} \ \times \ \mbox{Serum Creatinine (in mg/dL)}}](http://upload.wikimedia.org/math/4/6/e/46e61afd39d2a3acc66f456c33392c9e.png)

![\mbox{eGFR} = \mbox{186}\ \times \ \mbox{Serum Creatinine}^{-1.154} \ \times \ \mbox{Age}^{-0.203} \ \times \ {[1.212\ if\ Black]} \ \times \ {[0.742\ if\ Female]}](http://upload.wikimedia.org/math/2/a/f/2af94a4226aee0d827f876fde8f138c0.png)
![\mbox{eGFR} = \mbox{32788}\ \times \ \mbox{Serum Creatinine}^{-1.154} \ \times \ \mbox{Age}^{-0.203} \ \times \ {[1.212\ if\ Black]} \ \times \ {[0.742\ if\ Female]}](http://upload.wikimedia.org/math/d/b/9/db99b12cf04744ca85893735332b9534.png)
![\mbox{eGFR} = \mbox{170}\ \times \ \mbox{Serum Creatinine}^{-0.999} \ \times \ \mbox{Age}^{-0.176} \ \times \ {[0.762\ if\ Female]} \ \times \ {[1.180\ if\ Black]} \ \times \ \mbox{BUN}^{-0.170} \ \times \ \mbox{Albumin}^{+0.318}](http://upload.wikimedia.org/math/7/2/7/727fb222d37012663ab0c148d375dba6.png)
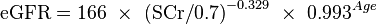
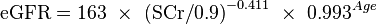
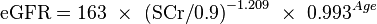
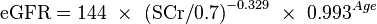
![\mbox{eGFR} = \mbox{141}\ \times \ \mbox{min(SCr/k,1)}^{a} \ \times \ \mbox{max(SCr/k,1)}^{-1.209} \ \times \ \mbox{0.993}^{Age} \ \times \ {[1.018\ if\ Female]} \ \times \ {[1.159\ if\ Black]} \](http://upload.wikimedia.org/math/4/6/b/46b8ff7c0e46ef484446555d2c23b423.png)




![\mbox{eGFR} = \mbox{exp}{(1.911+ 5.249/{Serum\ Creatinine} - 2.114/{Serum\ Creatinine}^2 - 0.00686 \ \times \ \mbox{Age} - {[0.205\ if\ Female]})}](http://upload.wikimedia.org/math/8/8/f/88f67e900e9c92f55e31c925b5ea3ab3.png)

 goes down. Also, even though the respiratory muscles are voluntary, you can't consciously control them when you're sleeping. So, how is respiratory rate altered & how is respiration controlled,
goes down. Also, even though the respiratory muscles are voluntary, you can't consciously control them when you're sleeping. So, how is respiratory rate altered & how is respiration controlled,




























