Kidney function tests
Kidney function tests are common lab tests used to evaluate how well the kidneys are working. See links below for details of how each test is performed:1.BUN
BUN stands for blood urea nitrogen. Urea nitrogen is what forms when protein breaks down.
A test can be done to measure the amount of urea nitrogen in the blood.
A test can be done to measure the amount of urea nitrogen in the blood.
How the Test is Performed
Blood is typically drawn from a vein, usually from the inside of the elbow or the back of the hand. The site is cleaned with germ-killing medicine (antiseptic). The health care provider wraps an elastic band around the upper arm to apply pressure to the area and make the vein swell with blood.Next, the health care provider gently inserts a needle into the vein. The blood collects into an airtight vial or tube attached to the needle. The elastic band is removed from your arm.
Once the blood has been collected, the needle is removed, and the puncture site is covered to stop any bleeding.
In infants or young children, a sharp tool called a lancet may be used to puncture the skin and make it bleed. The blood collects into a small glass tube called a pipette, or onto a slide or test strip. A bandage may be placed over the area if there is any bleeding.
How to Prepare for the Test
Many drugs affect BUN levels. Before having this test, make sure the health care provider knows which medications you are taking.Drugs that can increase BUN measurements include:
- Allopurinol
- Aminoglycosides
- Amphotericin B
- Aspirin (high doses)
- Bacitracin
- Carbamazepine
- Cephalosporins
- Chloral hydrate
- Cisplatin
- Colistin
- Furosemide
- Gentamicin
- Guanethidine
- Indomethacin
- Methicillin
- Methotrexate
- Methyldopa
- Neomycin
- Penicillamine
- Polymyxin B
- Probenecid
- Propranolol
- Rifampin
- Spironolactone
- Tetracyclines
- Thiazide diuretics
- Triamterene
- Vancomycin
- Chloramphenicol
- Streptomycin
How the Test Will Feel
When the needle is inserted to draw blood, some people feel moderate pain, while others feel only a prick or stinging sensation. Afterward, there may be some throbbing.Why the Test is Performed
The BUN test is often done to check kidney function.Normal Results
7 - 20 mg/dL. Note that normal values may vary among different laboratories.What Abnormal Results Mean
Higher-than-normal levels may be due to:- Heart attack
- Kidney disease,
- Liver failure
- Low protein diet
- Malnutrition
- Over-hydration
- Acute nephritic syndrome
- Atheroembolic kidney disease
- Diabetic nephropathy/sclerosis
- Epilepsy
- Goodpasture syndrome
- Hepatokidney syndrome
- Lupus nephritis
- Malignant hypertension (arteriolar nephrosclerosis)
- Secondary systemic amyloidosis
- Wilms' tumor
Risks
Veins and arteries vary in size from one patient to another and from one side of the body to the other. Obtaining a blood sample from some people may be more difficult than from others.Other risks are slight but may include:
- Excessive bleeding
- Fainting or feeling light-headed
- Hematoma (blood accumulating under the skin)
- Infection (a slight risk any time the skin is broken)
Considerations
For people with liver diseases the BUN level may be low even if the kidneys are normal.Alternative Names
Blood urea nitrogen2.Creatinine - blood
Creatinine is a breakdown product of creatine, which is an important part of muscle. This article discusses the laboratory test to measure the amount of creatinine in the blood.
How the Test is Performed
Blood is drawn from a vein, usually from the inside of the elbow or the back of the hand. The site is cleaned with germ-killing medicine (antiseptic). The health care provider wraps an elastic band around the upper arm to apply pressure to the area and make the vein swell with blood.Next, the health care provider gently inserts a needle into the vein. The blood collects into an airtight vial or tube attached to the needle. The elastic band is removed from your arm.
Once the blood has been collected, the needle is removed, and the puncture site is covered to stop any bleeding.
In infants or young children, a sharp tool called a lancet may be used to puncture the skin and make it bleed. The blood collects into a small glass tube called a pipette, or onto a slide or test strip. A bandage may be placed over the area if there is any bleeding.
How to Prepare for the Test
The health care provider may tell you to stop taking certain drugs that may affect the test. Such drugs include:- Aminoglycosides (for example, gentamicin)
- Cimetidine
- Heavy metal chemotherapy drugs (for example, Cisplatin)
- Kidney damaging drugs such as cephalosporins (for example, cefoxitin)
- Trimethoprim
How the Test Will Feel
When the needle is inserted to draw blood, some people feel moderate pain, while others feel only a prick or stinging sensation. Afterward, there may be some throbbing.Why the Test is Performed
The test is done to evaluate kidney function. Creatinine is removed from the body entirely by the kidneys. If kidney function is abnormal, creatinine levels will increase in the blood (because less creatinine is released through your urine).Creatinine levels also vary according to a person's size and muscle mass.
Normal Results
A normal value is 0.8 to 1.4 mg/dL.Females usually have a lower creatinine than males, because they usually have less muscle mass.
Note: Normal value ranges may vary slightly among different laboratories. Talk to your doctor about the meaning of your specific test results.



![eC_{Cr} = \frac { \mbox{(140 - Age)} \ \times \ \mbox{Mass (in kilograms)} \ \times \ [{0.85\ if\ Female}]} {\mbox{72} \ \times \ \mbox{Serum Creatinine (in mg/dL)}}](http://upload.wikimedia.org/math/4/6/e/46e61afd39d2a3acc66f456c33392c9e.png)

![\mbox{eGFR} = \mbox{186}\ \times \ \mbox{Serum Creatinine}^{-1.154} \ \times \ \mbox{Age}^{-0.203} \ \times \ {[1.212\ if\ Black]} \ \times \ {[0.742\ if\ Female]}](http://upload.wikimedia.org/math/2/a/f/2af94a4226aee0d827f876fde8f138c0.png)
![\mbox{eGFR} = \mbox{32788}\ \times \ \mbox{Serum Creatinine}^{-1.154} \ \times \ \mbox{Age}^{-0.203} \ \times \ {[1.212\ if\ Black]} \ \times \ {[0.742\ if\ Female]}](http://upload.wikimedia.org/math/d/b/9/db99b12cf04744ca85893735332b9534.png)
![\mbox{eGFR} = \mbox{170}\ \times \ \mbox{Serum Creatinine}^{-0.999} \ \times \ \mbox{Age}^{-0.176} \ \times \ {[0.762\ if\ Female]} \ \times \ {[1.180\ if\ Black]} \ \times \ \mbox{BUN}^{-0.170} \ \times \ \mbox{Albumin}^{+0.318}](http://upload.wikimedia.org/math/7/2/7/727fb222d37012663ab0c148d375dba6.png)
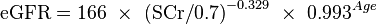
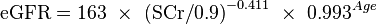
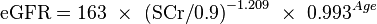
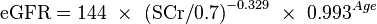
![\mbox{eGFR} = \mbox{141}\ \times \ \mbox{min(SCr/k,1)}^{a} \ \times \ \mbox{max(SCr/k,1)}^{-1.209} \ \times \ \mbox{0.993}^{Age} \ \times \ {[1.018\ if\ Female]} \ \times \ {[1.159\ if\ Black]} \](http://upload.wikimedia.org/math/4/6/b/46b8ff7c0e46ef484446555d2c23b423.png)




![\mbox{eGFR} = \mbox{exp}{(1.911+ 5.249/{Serum\ Creatinine} - 2.114/{Serum\ Creatinine}^2 - 0.00686 \ \times \ \mbox{Age} - {[0.205\ if\ Female]})}](http://upload.wikimedia.org/math/8/8/f/88f67e900e9c92f55e31c925b5ea3ab3.png)
